Examining the impact of psychological distress on soldiers’ spinal injuries
on October 17th, 2012 No Comments
 The latest issue of The Spine Journal is devoted to casualties of war and includes some interesting insight into how the emotional stress of combat can impact soldiers’ spine injuries.
The latest issue of The Spine Journal is devoted to casualties of war and includes some interesting insight into how the emotional stress of combat can impact soldiers’ spine injuries.
A key finding reported on in the issue is that non-battle spinal pain is a leading cause of medical evacuation for those deployed in Iraq and Afghanistan. Among other noteworthy findings, as outlined in a journal release:
- There have been 10 times as many long-term spinal-pain casualties unrelated to battle as blast injuries
- 60 percent of veterans seeking care for spine problems have serious continued psychological distress
- Less than one percent of military-aged Americans serve in the military (compared to nearly 50 percent during World War II), which means that veterans’ burdens after combat are now far less visible to the general public
In the release, Stanford orthopedic surgeon and journal editor-in-chief Eugene Carragee, MD, who wrote several pieces on spinal injuries for this issue and has done two tours of duty in Iraq himself, comments:
While some of the findings in this special issue are new and specific to these long wars—such as the devastating effects of IED blasts—it’s clear that we need to re-learn some very old lessons about war… We repeatedly send young people into combat to experience the worst psychological stressors possible, push them beyond endurance, and yet on the home front there is little to no collective understanding of the wars they fought or the experiences of deployment and combat. Veterans seeking care for spine problems at home are shown to have continued serious psychological distress, associated with exposure to combat. This is a serious public health issue that will continue for many years.
Previously: Stanford and other medical schools to increase training and research for PTSD, combat injuries, As soldiers return home, demand for psychologists with military experience grows, Helping brain-injured soldiers return – safely – to the battlefield and Are veterans with PTSD at higher risk for medical illnesses?
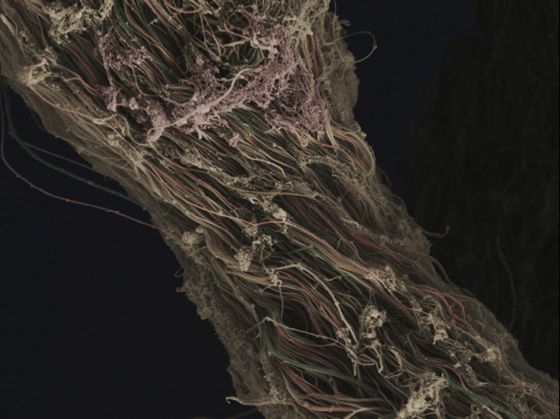
Photo by Staff Sgt. Stacey Haga/U.S. Air Force