Stanford computer scientist shows stem cell researchers the power of big data
on May 7th, 2013 No Comments
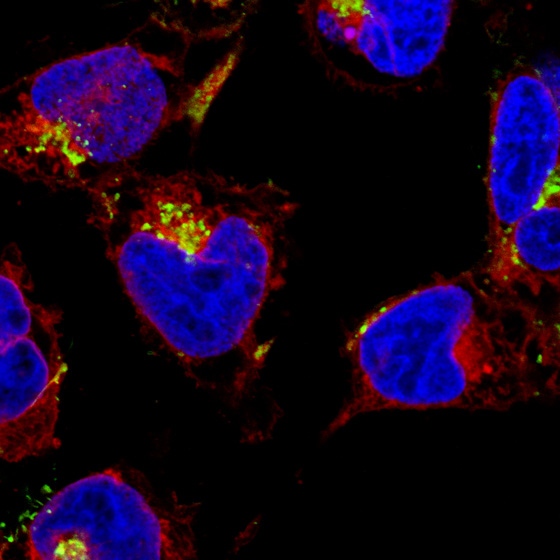
Not long ago, Stanford computer scientist Debashis Sahoo, PhD, told investigators at the Stanford Institute for Stem Cell Biology and Regenerative Medicine that in a few seconds he could find many of the important stem cell genes that the researchers were used to finding only after spending millions of dollars and years in the lab. “We laughed and said, ‘That’s impossible,’” recalls Irving Weissman, MD, director of the institute, in a recent video. But Weissman went ahead and gave Sahoo information about two key genes - and within a few seconds, Sahoo had used his desktop computer to scour the world’s public gene databases, analyzed that information with the computer algorithm he had designed, and come up with over a dozen genes new genes that were involved in the development of certain kinds of cells. That search, Weissman estimates, saved his team a decade of work and about $2.5 million.
More details are shared in the video above. And as a reminder, big data - and the ways in which people like Sahoo are mining through vast amounts of publicly available information to further research and advance health care - is the focus of a Stanford/Oxford conference being held here later this month.
Previously: Atul Butte discusses why big data is a big deal in biomedicine and Mathematical technique used to identify bladder cancer marker

 UPDATE 01-30-10: In writing about what seems to be a clear case of medical abuse I did not note that there are legitimate scientists who continue to investigate the use of bone marrow cells as a vehicle for heart repair. My apologies to them. However, these therapies are still in the research stage and patients should only get them as part of a controlled clinical trial. The problem in differentiating research that is legitimate from that which isn’t only highlights the need for a certification system for stem cell treatments.
UPDATE 01-30-10: In writing about what seems to be a clear case of medical abuse I did not note that there are legitimate scientists who continue to investigate the use of bone marrow cells as a vehicle for heart repair. My apologies to them. However, these therapies are still in the research stage and patients should only get them as part of a controlled clinical trial. The problem in differentiating research that is legitimate from that which isn’t only highlights the need for a certification system for stem cell treatments. The New York Times recently
The New York Times recently 




